If you’ve ever found yourself dealing with strange symptoms after a meal—maybe hives, bloating, or an itchy rash—you know how worrying and confusing it can be. The very first thing to do, before any tests, is to start keeping a food diary. It sounds simple, but this is the single most important step to gather the clues you need to figure out what's going on.
When you or your child has a reaction after eating, the immediate question is always, "Why?" Unexplained hives, stomach cramps, or a sudden eczema flare-up can be really unsettling. The path to a proper diagnosis doesn't start in a clinic, but right at your kitchen table. You need to become a bit of a detective, and your best tool is a food and symptom diary.
Imagine a parent in Manchester who notices their toddler's eczema gets worse a day or two after having yoghurt. The actionable first step is to jot this down: "Monday: yoghurt for breakfast. Tuesday evening: red, itchy patches on arms." By creating this simple record, a pattern starts to take shape. This kind of practical insight is invaluable when you eventually speak to a healthcare professional.
It’s crucial to get your head around the two main types of adverse food reactions. They involve different parts of your body's defence system and need different approaches to get answers.
Understanding this difference is a key actionable insight, as it helps you know what to expect from testing. A blood test can spot IgE sensitisation, but an intolerance might need a completely different approach, like an elimination diet supervised by a professional.
A detailed food and symptom diary is the most powerful tool you have at the start. It turns vague worries into solid information you can discuss with your GP, making that appointment much more effective.
If you're going through this, you're far from alone. Food allergy rates in the UK have shot up dramatically over the last decade, jumping from 0.4% to 1.1% between 2008 and 2018. The increase is particularly stark in young children, with 4.0% of under-5s now affected. This really highlights why getting clear, accessible information early on is so important. You can learn more about these allergy statistics and what they mean for UK families.
This is where knowing your options becomes empowering. The traditional route involves seeing your GP for a potential referral, but gathering your own preliminary data can speed things up. Taking charge gives you the evidence you need for a much more productive conversation with your doctor.
For example, using one of our at-home tests fits perfectly into this initial fact-finding stage. They offer clear, lab-verified insights from home, so you can walk into your GP appointment armed with a detailed symptom diary and concrete results, ready to take the next step.
Navigating your testing options can feel overwhelming. To make it clearer, let's compare the typical journey through the NHS with the more direct route of private at-home testing.
Here’s a quick look at the typical journey for getting an allergy test through the NHS versus using a private at-home service like Repose Healthcare.
| Milestone | Typical NHS Pathway | At-Home Testing Pathway |
|---|---|---|
| Initial Concern | You notice symptoms and start a food diary. | You notice symptoms and start a food diary. |
| First Contact | Book a GP appointment, which may have a waiting time. | Order a test kit online, which arrives in a few days. |
| Sample Collection | If referred, you'll have a blood test at a clinic or hospital. | Collect a simple finger-prick blood sample at home. |
| Testing | Sample is sent to an NHS lab. Results go back to your GP. | Mail your sample back to an accredited lab in the provided envelope. |
| Receiving Results | Wait for your GP to receive and interpret the results, then book a follow-up appointment. | Receive your results securely online within days. |
| Next Steps | Discuss results with your GP to determine the next steps, like a specialist referral. | Share your results with your GP for a more informed discussion and faster decision-making. |
As you can see, both paths aim for the same goal: getting clarity on your symptoms. An at-home test can provide you with valuable, data-driven insights much faster, allowing you to have a more targeted and efficient consultation with your GP when you're ready.
When your food diary starts pointing fingers at a potential allergy, your GP might suggest a formal clinical test to get a proper look at what's going on. These tests take you from suspicion to scientific evidence, helping to nail down exactly what’s causing your symptoms.
Let's break down the main options you're likely to come across.
One of the most common methods you'll encounter is the Skin Prick Test (SPT). It's a very straightforward procedure done right there in the clinic. A clinician will place tiny droplets of liquid, each containing a different allergen, onto your forearm or back. They then make a tiny scratch through each drop, letting a minuscule amount of the substance get just under the skin.
If you’re allergic, your body kicks into gear and releases histamine in response to that allergen. For instance, if you're allergic to milk, a small, red, itchy bump called a wheal will pop up at the milk scratch site, usually within 15-20 minutes. It looks a bit like a mosquito bite and serves as a clear visual sign of sensitisation.
An SPT is brilliant because it's fast and gives you answers on the spot. But, it's not the right fit for everyone. If you have a severe skin condition like eczema, or if you can't stop taking antihistamines (which would block the reaction), your doctor will need to look at a different approach.
Another cornerstone of allergy diagnosis is the Serum Specific IgE Blood Test. This involves analysing a small sample of your blood to measure the amount of specific Immunoglobulin E (IgE) antibodies. Think of these as the 'allergy antibodies' your immune system produces to fight off what it sees as a threat.
So, if you react to prawns, a blood test can count the exact number of IgE antibodies that are programmed to attack prawn proteins. A higher level of these specific antibodies is a strong indicator that you are sensitised to that food. This is the very same trusted, lab-based technology we use in our at-home allergy tests, giving you a convenient way to gather this crucial information yourself.
A huge advantage of the IgE blood test is how convenient and safe it is. It can be done on anyone, regardless of their skin condition or what medications they're on, and it just needs one small blood sample. To get a better idea of how this works from the comfort of your home, check out our guide to finger-prick blood tests at home.
This one is considered the gold standard for diagnosing a food allergy. The Oral Food Challenge (OFC) is the most definitive test there is, but it's always done under strict medical supervision in a hospital or specialist clinic because of the risk of a severe reaction.
During an OFC, you’ll be given gradually increasing amounts of the food you’re suspected to be allergic to. For example, if a peanut allergy is suspected, you might be given a tiny crumb of a peanut to start, followed by larger amounts over several hours while medical staff watch you closely for any sign of a reaction. If you can eat a full, normal portion with zero symptoms, the allergy is officially ruled out.
An OFC is usually brought in when other test results are a bit fuzzy or to check if someone has outgrown a childhood allergy. It gives a real-world, yes-or-no answer, but because of the potential risks, it's saved for very specific situations.
It's absolutely crucial to know that a positive skin prick or blood test shows sensitisation, which isn't the same as a clinical allergy. Sensitisation just means your body makes IgE antibodies to a food; you might be able to eat it without any problems at all. A true allergy diagnosis needs both a positive test and a clear history of symptoms after eating the food.
This flowchart gives a good overview of the typical first steps for investigating a suspected food allergy here in the UK.
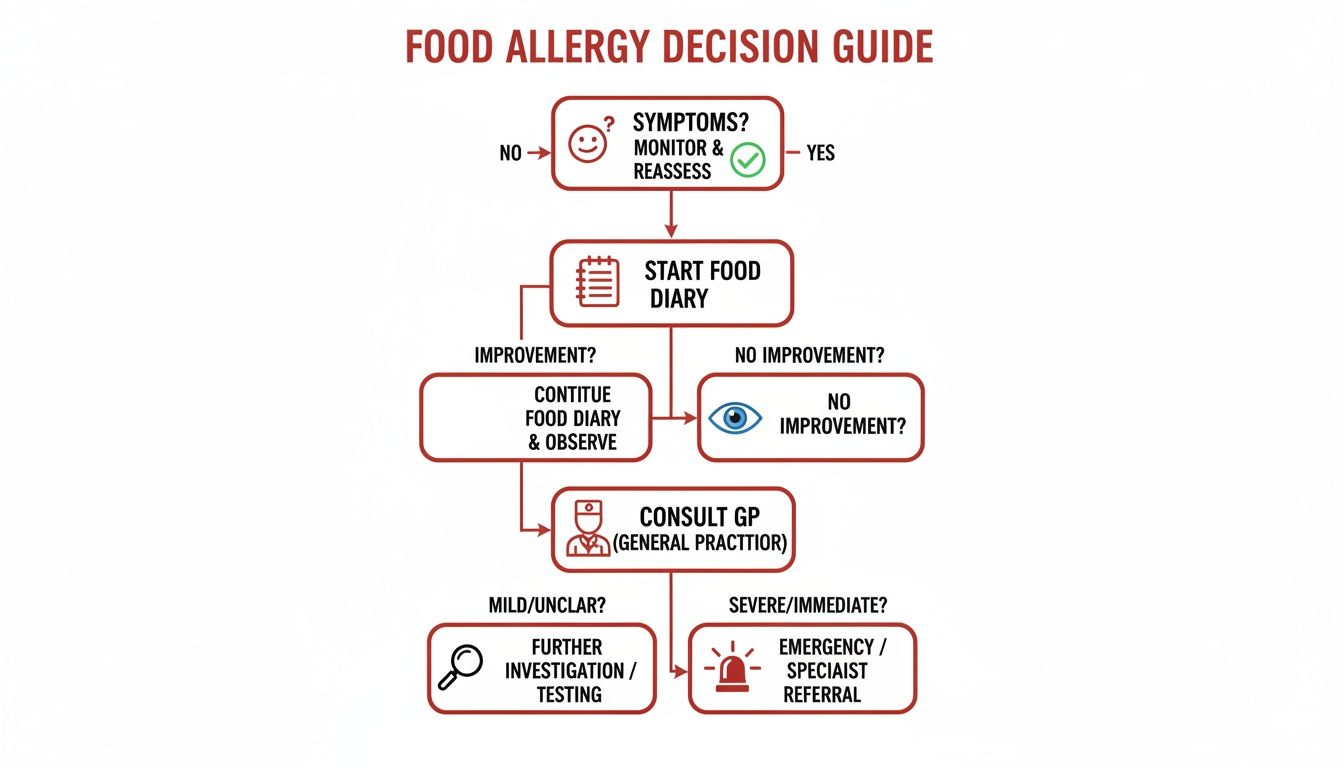
As you can see, the journey always begins with you recognising your symptoms and keeping a record. That groundwork is what makes for a really productive conversation with your GP.
The right test for you boils down to your personal situation, your symptoms, and your medical history. Your GP or an allergy specialist will guide you down the most sensible path.
Each test offers a vital piece of the puzzle. By understanding what each one involves and what the results really mean, you can work much more effectively with your doctor to get the answers you need.
Let's face it, waiting for clinic appointments can be a real drag. At-home allergy testing has become a popular and reliable way for people across the UK to get some initial data without the long waits. It puts you in the driver's seat, letting you collect a sample right from your own home, whenever it suits you. This is a game-changer for busy parents, professionals, or anyone who just wants clear, quick insights into what might be causing their symptoms.

The whole process is straightforward and discreet. Imagine a parent in Ireland wanting to investigate their child's recurring hives without taking time off work for multiple appointments. With an at-home kit, they can collect a simple sample at the kitchen table over the weekend and have results in a few days. It’s a convenient first step to understanding potential triggers.
Accessible testing has never been more important. Recent analysis shows that around 3% of the UK population is at risk of life-threatening IgE-mediated reactions. Over a 20-year period, hospitalisations for severe food anaphylaxis shot up from 1.23 to 4.02 per 100,000 people annually, making up nearly a third of all anaphylaxis admissions. These numbers really highlight the value of identifying potential allergens early and accurately. You can explore the research from the Food Standards Agency to see the full picture.
First things first, you need to choose the right test. Different panels are designed to look for specific groups of allergens, so it’s worth taking a moment to think about what you're trying to find out. Are you worried about a whole range of potential triggers, or do you have a few specific foods in mind?
For example, if your symptoms are broad and unexplained, our ALEX Allergy Test for 300 allergens is an excellent starting point. It screens for a wide array of common food allergens, giving you a really thorough overview. It’s the ideal choice when you’re not sure where to begin and want to cast a wide net.
On the other hand, if your food diary points strongly towards a certain category, a more focused panel might be better. For instance, if you suspect nuts or seafood are the issue, you could select a test that specifically targets those allergens. This tailored approach lets you investigate your primary suspects much more efficiently.
Once your Repose Healthcare kit arrives, you’ll find everything you need inside, including clear instructions. The process involves collecting a small blood sample using a simple finger-prick method. This might sound a bit daunting, but a few practical tips can make it a completely smooth experience.
Here’s an actionable insight to get a good blood flow:
When you're ready, use the provided lancet on the side of a fingertip on your non-dominant hand—it’s usually less calloused. Gently massage your finger from the base to the tip to help the drops form, and collect them in the vial.
The key is to be relaxed and prepared. Lay everything out on a clean surface before you start. Following the simple warming tips can make a huge difference, ensuring you get enough of a sample on the first try without any fuss.
After you've collected your sample, the next step couldn't be simpler. Just seal the vial as instructed, place it in the secure, prepaid return envelope, and pop it in the post. You don't need to worry about postage or special handling; it’s all taken care of.
Your sample goes directly to one of our fully accredited UK laboratories. These are the same labs used by GPs and hospitals, so you can be confident your test is processed to the highest clinical standards. This ensures the results you receive are not just fast, but also robust and reliable.
The whole process is designed for convenience and accuracy, bridging the gap between your initial concerns and a productive, data-led conversation with your doctor. To learn more about how this fits into your wider health journey, have a read of our detailed guide on allergies and the role of self-testing. Getting these initial insights can fast-track your path to clear answers and an effective management plan.
Getting the notification that your allergy test results are in can bring a mix of relief and nervousness. The report itself is often full of numbers, technical terms, and classifications that don't immediately make sense. But don't worry—learning to decode this information is the first real step toward creating a practical action plan for your health.
The key figure you'll see is your specific IgE (sIgE) level, usually measured in kiloUnits per litre (kU/L). You can think of IgE as your body’s own "allergy antibodies." For example, when your immune system wrongly flags a harmless protein from a peanut as an invader, it churns out these sIgE antibodies specifically to fight it.
A blood test simply measures how many of these specific antibodies are circulating for each allergen tested. A higher sIgE number for a certain food generally points to a stronger degree of sensitisation. This is the core data that reveals what your body is primed to react to.

Your results will sort each allergen into one of two camps: 'positive' or 'negative'.
A negative result is straightforward. It means no significant sIgE antibodies were found for that food, making an IgE-mediated allergy highly unlikely. It’s often a big relief.
A positive result, on the other hand, needs a little more context. It confirms that you are sensitised to that food. Essentially, your immune system has built the tools (the sIgE antibodies) to launch a reaction. This is a critical piece of the puzzle, but it’s not the same as having a confirmed clinical allergy.
If you take one thing away from this, let it be this: sensitisation does not automatically equal a clinical allergy. This is the single most important concept to grasp.
Sensitisation means your body has the potential to react. A clinical allergy only exists if you actually experience symptoms after eating the food.
Let’s look at a practical example. Imagine two friends, Sarah and Tom, both get a positive test result for peanut sIgE.
This distinction is absolutely vital. You should never cut foods out of your diet based on a test result alone, particularly if you've been eating them without any issues. Doing so can lead to needless dietary restrictions and a lot of unnecessary anxiety.
Your test results are a crucial clue, not the final verdict. The real picture emerges when you combine the lab data with your real-life experiences and symptoms.
A Repose Healthcare results dashboard is designed to make this clear. It will show the specific IgE value for each allergen alongside its classification, so you can easily see what your body is sensitised to. To get an idea of the breadth of our most comprehensive panel, you can explore the ALEX Allergy Test for 300 allergens.
Labs often provide a reference range to help contextualise the numbers. While every lab is slightly different, here is a general guide to what the levels might indicate.
This table gives you a general idea of how IgE levels are classified. Remember, these are just indicators; the real meaning comes from discussing them with a doctor in the context of your symptoms.
| IgE Level (kU/L) | Class | Antibody Level | What This May Indicate |
|---|---|---|---|
| < 0.35 | 0 | Undetectable | An IgE-mediated allergy is highly unlikely. |
| 0.35 – 0.69 | 1 | Low | Low-level sensitisation; may or may not be clinically relevant. |
| 0.70 – 3.49 | 2 | Moderate | A definite level of sensitisation. Correlation with symptoms is key. |
| 3.50 – 17.49 | 3 | High | Strong sensitisation. A higher likelihood of clinical symptoms. |
| 17.5 – 49.9 | 4 | Very High | Very strong sensitisation. Clinical allergy is highly probable. |
| 50 – 99.9 | 5 | Very High | Indicates a very significant level of sensitisation. |
| > 100 | 6 | Extremely High | Represents the highest level of sensitisation measured. |
It's tempting to focus only on the numbers, but a "high" value for a food you eat without issue is less concerning than a "low" value for a food that makes your lips tingle. Context is everything.
So, what should you do now? Your results are a powerful tool for a productive conversation with your GP or a specialist allergist. Please, never make major dietary changes based on test results alone.
Here's an actionable plan:
Your at-home test provides the precise data you need to kickstart that conversation, putting you in the driver's seat of your own health journey.
Sometimes, a blood test for IgE antibodies just doesn't give you the full picture. What if your results come back clear, but you're still wrestling with symptoms like bloating, brain fog, or eczema? This is often where a non-IgE mediated food intolerance comes into play, and an elimination diet becomes an incredibly powerful diagnostic tool.
Think of an elimination diet less like a clinical test and more like a real-world investigation. It’s a methodical process where you remove certain foods to see if your symptoms ease up, and then carefully reintroduce them one by one to see what triggers a reaction. Your body's direct feedback is the guide.
This approach is particularly good for identifying those delayed reactions that standard allergy tests simply can't pick up. For instance, you might suspect gluten is behind your persistent fatigue and headaches, even after a coeliac test comes back negative. By cutting out gluten for a few weeks and noticing a definite improvement, you gain invaluable insight into a possible non-coeliac gluten sensitivity.
Starting an elimination diet isn't about randomly cutting out foods. It's a structured experiment that needs careful planning to be both safe and effective.
The first actionable step is the elimination phase. This means you completely remove one or more suspected trigger foods from your diet for a set period, usually 2-4 weeks. The idea is to give your body a 'clean slate' so you can accurately observe what happens when you bring that food back in. Some of the most common foods to remove include:
During this time, keeping a detailed food and symptom diary is non-negotiable. You have to meticulously track everything you eat and how you feel, noting any changes in energy levels, digestion, skin, or mood.
Crucial Safety Note: Elimination diets should always be supervised by a registered dietitian or your GP, especially for children or anyone with complex health conditions. Professional guidance is vital to avoid nutritional deficiencies and ensure the reintroduction phase is done safely.
So, you've completed the elimination period and your symptoms have noticeably improved. Great! Now comes the reintroduction or challenge phase. This is where you get your answers, but it has to be done slowly and methodically.
You'll reintroduce just one food group at a time. Start with a tiny amount on the first day, then gradually increase the portion over the next two days, all while keeping a close eye out for any returning symptoms.
Let's use dairy as a practical example:
After this three-day test, you'll wait another few days to see if any delayed reactions pop up. If symptoms come back, you've very likely found a trigger. If not, you can probably assume that food is safe and move on to the next one on your list.
This careful, one-by-one process is the only way to avoid confusion and confidently pinpoint exactly what’s causing the problem. Alongside this, it's essential to implement safe food handling practices to avoid accidental exposure, so take the time to learn about preventing cross-contamination in your kitchen. This becomes especially important if you're managing a household with different dietary needs.
Ultimately, an elimination diet is a highly personal journey. It empowers you to understand your body's unique responses and gives you the clear, definitive answers needed to build a diet that helps you feel your absolute best.
Trying to get to the bottom of a suspected food allergy can feel overwhelming. With so much information out there about different tests, it's easy to get confused. We get a lot of questions about the process, so let's clear up some of the most common ones.
An at-home IgE blood test, like the ones from Repose Healthcare, is a crucial first step in the diagnostic journey. It works by identifying sensitisation to specific foods—that is, whether your body produces allergy-related antibodies (IgE) to them.
A positive result is a strong clue, but a formal diagnosis only comes when a doctor connects that lab data with your specific symptoms. Think of our tests as providing the vital evidence you need to have a really productive conversation with your GP.
One isn't necessarily 'better' than the other; they're simply different tools for different scenarios. A skin prick test is done in a clinic and gives you results very quickly, but its accuracy can be skewed by common medications like antihistamines.
An IgE blood test, on the other hand, isn’t affected by most medications and can be done from anywhere. It gives a precise measurement of the allergy antibodies circulating in your blood. Often, an allergist will look at results from both types of tests to build a complete picture. This is why starting with a reliable at-home blood test can be so helpful.
A key advantage of a blood test is its reliability. Because it is not affected by antihistamines, you get a clear and accurate measurement of your body's sensitisation level without having to stop your usual medications.
Modern IgE blood tests and skin prick tests are very accurate at spotting sensitisation. It’s important to remember, though, that a positive result doesn't automatically mean you'll have an allergic reaction every time you eat that food.
Tests from accredited labs, like those used by Repose Healthcare, provide clinically reliable results you can trust. This gives you a solid foundation for discussing your symptoms with a healthcare professional and figuring out the right next steps for you.
It's completely understandable to feel stressed when you see your child having a reaction. The first and most important thing to do is start a detailed food and symptom diary. Note down everything they eat and any reactions they have—this is an invaluable tool for spotting patterns.
The next step is to book an appointment with your GP. They are the best person to assess the situation and decide what needs to happen next, whether that’s a referral to a specialist or ordering specific tests. When it comes to your child's health, getting professional medical guidance is absolutely essential.
Ready to take control and get some clarity? Repose Healthcare offers a range of at-home allergy and coeliac tests that deliver fast, lab-verified results from a simple finger-prick sample. Explore our tests and find the right one for you at https://reposehealthcare.co.uk.